Africa is falling behind in its quest to meet the 2030 Sustainable Development Goal (SDG) targets for maternal and newborn health, with fresh evidence showing that maternal mortality remains alarmingly high in West and Central African countries.
The new 2025 report of the Lancet Countdown to 2030 for women's, children's, and adolescents' health: tracking progress on health and nutrition highlights a troubling slowdown in progress across the continent, prompting urgent calls by health experts for stronger data systems to inform policy and investment in reproductive and maternal health.
Speaking during the Country Annual Meeting (CAM 2025) themed producing reliable national and subnational health statistics with a focus on maternal, newborn, child and adolescent health and nutrition Dr Hillary Kipruto, a health systems expert from the World Health Organisation (WHO) Kenya, emphasised the urgent need for governments to prioritise data-driven action to improve outcomes for women, children, and adolescents.
“We’ve made progress in some countries, yes. But the truth is, the progress is uneven. Even within individual countries, maternal mortality remains a crisis,” he said.
The report, compiled by Countdown to 2030 in partnership with the African Population Health Research Center (APHRC), shows maternal mortality ratios (MMRs) in several West and Central African nations remain among the highest globally, exceeding 500 deaths per 100,000 live births. The target under SDG 3 is to reduce global MMR to less than 70 by 2030.
“COVID-19 derailed progress, but so did armed conflict, weak health systems, and poor governance,” said Cheikh Mbacké Faye, Director of APHRC’s West Africa office. “Some countries, particularly in the Sahel and parts of the Democratic Republic of Congo, have seen reversals. Health systems there are struggling to deliver even basic services.”
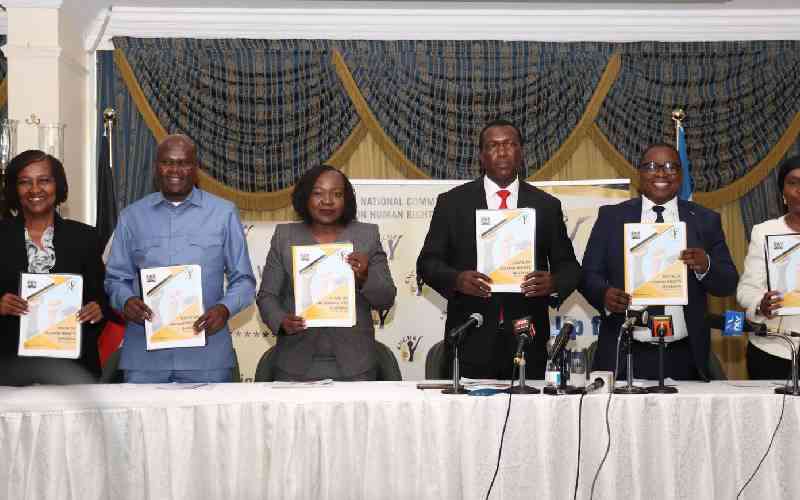
The workshop, hosted by Kenya’s Ministry of Health in collaboration with UNICEF, WHO, and the Gates Foundation, explored practical solutions for rebuilding data systems. A major theme was the need for better subnational data – information from the district and community levels where care is delivered and lives are lost or saved.
Dr Abdihamid Ibrahim Ahmed Regional Health Systems and Primary Healthcare Coordinator – UNICEF emphasised that far too many women and children remain overlooked in health systems—especially at the sub-national and district levels, where essential services are delivered, progress is tracked, and funding decisions are made.
- Silent killer: Postpartum bleeding still claims ten mothers every day
- Deadlier than crashes: How bleeding crisis is haunting delivery rooms
- Why experts are pushing for breastfeeding, warn against formula feeding
- Mothers at risk as bleeding detectors run out
Keep Reading
“In today’s reality of shrinking budgets and stretched resources, the pressure to achieve more with less has never been greater,” he said. “This makes routine health data not just a luxury, but a lifeline. As many have rightly pointed out, what isn’t counted can’t be improved—and what isn’t measured simply cannot be achieved.”
“Routine data isn’t just a nice-to-have anymore—it’s a lifeline. It helps us identify who’s being left behind and allows us to better allocate limited resources.”
Dr Kipruto notes that DHS surveys have traditionally provided reliable population-level data on maternal and child health, but now face uncertain future funding. “The United States government has been the biggest funder of this work, but domestic investment in health information systems remains very low across Africa,” he said.
Kipruto outlined four pillars for strengthening data systems: robust governance frameworks, functional systems for data generation and storage (such as the widely adopted DHIS2), enhanced analytical capacity within ministries, and above all, the political will to translate evidence into action.
“It’s not enough to have beautiful infographics and reports. If the data doesn’t lead to concrete actions at the national and local levels, then we’ve failed,” he said.
According to the report, most maternal deaths in Africa stem from preventable causes such as hemorrhage, hypertensive disorders, infections, and unsafe abortions.
These deaths are often linked to delays in accessing quality care—delays caused by poor infrastructure, understaffed facilities, and lack of skilled birth attendants.
In addition, the report warns that adolescent pregnancy and limited access to contraception continue to drive poor reproductive health outcomes. In Sub-Saharan Africa, nearly 1 in 5 teenage girls give birth before the age of 18, exposing them to higher risks of maternal mortality and school dropouts.
Despite the grim statistics, experts pointed to pockets of progress. Rwanda and Ethiopia have made strides in reducing maternal deaths through strong political commitment, investment in community health workers, and decentralization of services. These countries are seen as models of how data-informed policies can yield real improvements.
“Data must serve the people. And that means we need to build the capacity of district health teams to use the data they collect,” said Dr Ahmed. “Perfection cannot be our starting point—we must work with the data we have and improve it as we go.”
At the heart of the discussions was a shared sense of urgency. With just five years to go before the SDG deadline, and maternal health outcomes stagnating or worsening in some countries, delegates agreed that the time to act is now.
“Health systems must be ready to respond not only to pandemics but to everyday emergencies in childbirth,” said Kipruto. “That means training health workers, equipping facilities, and investing in governance and leadership.”
In many African countries, health budgets still fall far short of the 15 per cent Abuja target set two decades ago. The share of those budgets allocated to data and monitoring is even smaller—often less than 1 per cent.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.